“It’s completely normal to be bleeding everyday for months … it will work itself out!” THIS WAS A QUOTE TOLD TO A WOMAN WHO CAME TO ME WITH PCOS.

PCOS or Polycystic Ovary Syndrome is the most common endocrine (hormone disorder). 10% of the female population, across all racial and ethnic backgrounds have PCOS. Women with PCOS usually come to me after they have already developed the following symptoms and diagnosis associated with the syndrome:
- Acne
- Hirsutism (excessive growth of dark or coarse hair in a male-like pattern)
- Obesity
- Autoimmune Disease – most notably Hashimotos
- infertility
- menstrual irregularities
- pre-diabetes
- heart disease
- fatty liver disease
These women have been told to lose weight so they over exercise, under-eat, lose 20-30 lbs and then fall off the bandwagon because let’s be honest, starving yourself IS NOT SUSTAINABLE or at the root of the metabolic dysfunction of PCOS. Many PCOS women walk around disheartened and worried about their future health, whether they’ll ever become Mom’s, blaming themselves for the crippling symptoms and thinking if they just had more willpower they would look and feel like their friends. It is heartbreaking and unacceptable that PCOS women aren’t given a comprehensive look at their overall health picture. PCOS women need help in understanding what is causing this cascade of symptoms they experience and they deserve to be given concrete, evidence based protocols to support their health.
 . I had the pleasure of interviewing Dr. Gersh on this subject – check out the episode on SHE Talks Health here, or click the link below.
. I had the pleasure of interviewing Dr. Gersh on this subject – check out the episode on SHE Talks Health here, or click the link below.What is PCOS? And how is PCOS diagnosed?
PCOS or PolyCystic Ovary Syndrome is a collection of symptoms that affects the entire metabolic, endocrine, immune, gut, cardiovascular systems of the female body. There have been some disagreements about the official symptoms needed to reach a diagnosis – which is one reason why you might be confused as to why one doctor told you that you have PCOS and another disagreed. (YES this happens to my clients!)
The definition that I personally ascribe to is from the Androgen Excess and PCOS Society (PDF) which says that a woman has PCOS if she has the following:
- Hyperandrogenism
- Irregular/missing cycle and/or ovarian dysfunction
- The exclusion of related disorders
Let’s break that down, shall we?
Hyperandrogenism – what is that, Sophie?!
HYPER (meaning – high, beyond, excessive) ANDROGEN (“male” sex hormones, most commonly Testosterone but also DHEA-S) ISM – A medical condition or a disease resulting from or involving some specified thing.
So Hyper-androgen-ism is an excessive amount of male sex hormones – this can be determined one of two ways. It can be determined by measuring your androgens on a blood test with your doctor or it can be shown in symptoms associated with Androgen excess – such as Hirsutism, acne, thinning hair on the scalp.
Women also need one of the following two thing to qualify for PCOS diagnosis through AE PCOS SOCIETY:
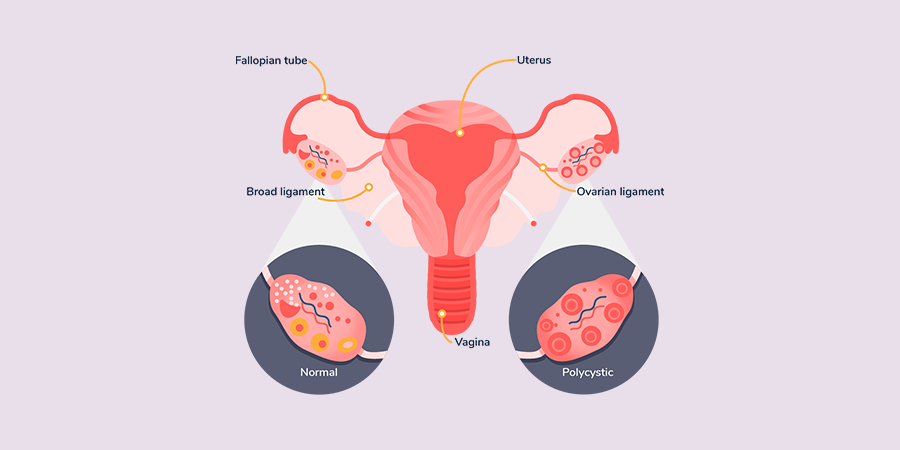
An irregular or completely missing menstrual cycle AND / OR Polycystic ovaries.
Polycystic ovaries are determined via ultrasound by showing that your ovaries contain lots of small follicles (these are not the same thing as ovarian cysts).
You would think from the name “Poly Cystic Ovary Syndrome” that Poly Cystic Ovaries would be the single deciding factor but it’s not! You truly have to consider the excess “male” hormones as well and the lack of, or irregular menses.
Dr. Lara Briden outlines in her book, The Period Repair Manual, why women can develop “Poly Cystic Ovaries”. She states:
“If you progress normally to ovulation… then one of your follicles will become dominant and larger than the others and will suppress the others the rest of that cycle. If you do not progress to ovulation (as occurs with PCOS) then you will not form a dominant follicle and suppress the others. Instead, the other follicles will keep growing just a little bit, and you will end up with many small undeveloped follicles. The problem with that is you did not ovulate and that led to higher than normal follicles (at least for that month!) There is no reason to think your ovaries will always look that way. Ovaries are dynamic and they change…”
PCOS is a diagnosis of exclusion
The doctor technically must rule out rare disorders like Cushing’s Syndrome and Adrenal Hyperplasia before officially diagnosing you with PCOS. This is why it is so crucial that you go to a doctor who can actually diagnose you properly so you know what you are dealing with.This is important because:
This means that PCOS can not be diagnosed by ultrasound or any one particular test because it is a syndrom, meaning “a collection of signs and features, where no single test is diagnostic.” PCOS, according to AE PCOS Society is the cumulation of Hyperandrogenism, plus irregular periods and/or polycystic ovaries as well as exclusion of related disorders. Being told you have PCOS when you don’t could lead to a lot of treatments and worry. Work with your doctor to get the correct diagnosis. This is part of being a health advocate. I wish it wasn’t so complicated but honestly sometimes we just have to have these conversations with our providers so we can truly understand what is happening with our unique bodies. If your provider isn’t willing to explain the methodology behind a diagnosis, please consider finding a new provider.What are the root causes of PCOS?
According to Dr. Gersh, “on a molecular level, the very root cause of PCOS is a problem with the process of aromatization.” Say, what now!?
Poor Aromatization means poor conversation from testosterone to estrogen. Did you know that the bulk of your estrogens come from testosterone?! Pretty crazy right? When women have poor aromatization it can result in not enough estrogen and too much testosterone.
To make matters worse, the body is on a feedback loop where the brain THINKS the body needs more estrogen and it KNOWS that estrogen is converted from Testosterone so it sends a request to create more Testosterone….which you guessed it – leads to hyperandrogenism because the body can’t convert Testosterone to Estrogen efficiently.
This poor aromatization causes all the facial hair & acne and loss of hair on the top of the scalp that women with PCOS often experience.
But poor aromatization has an even more sinister trickle down effect to many other organ systems in the body, because there are estrogen receptors in every organ in your body. This means that various organ systems are working suboptimally. For example, low estrogen causes circadian rhythm dysfunction (your sleep/wake cycle) which in turn exacerbates insulin resistance, weight gain, contributes to diabetes and heart disease (all conditions associated with PCOS). Circadian rhythm dysfunction further increases androgens which promotes even more acne, hirsutism etc. All of this can trigger downstream inflammation & GI issues which also exasperate PCOS symptoms.
What lifestyle interventions can you make to support PCOS?
There are MANY but here are my top three to get started with:

Reset your Master Clock

Heal the Gut

Eat For Your Hormones
Let’s go into each one shall we?
RESET THE MASTER CLOCK
This is talking about making sure your body is on the proper sleep/wake cycle aka going to bed at 10pm and waking up at 6am. We used to wake up with the sun and go to sleep with the sun but modern technology, housing, blue light, Netflix, stress and jobs in front of computers have drastically changed that. In order for our complex biological systems to work efficiently we need to get back to basics. I wrote an article a while back about how to get a good night’s sleep that I highly recommend reading.
In addition to this article, I would add that women with PCOS tend to have low melatonin levels and higher cortisol levels which makes it very difficult to sleep. You can try supplementing with melatonin, Dr. Gersh outlines this very specifically in her PCOS SOS book.
Before supplementing, I’m always a fan of testing, not guessing, to make sure you actually need a supplement for your unique body. For sleep, in addition to everything I wrote in my previous blog, I’m also a very big fan of the circadian rhythm blend, adrenal blend and parasympathetic blend from Vibrant Blue Oils. They also have a blood sugar support kit that may interest you. You can check out the interview I did with Jodi Cohen, the Founder on how these aren’t your typical essential oils. I also really like www.earthing.com blankets and CBD for extra sleep support.
SUPPORT THE GUT
Gut dysbiosis or an overgrowth of bad bacteria to good bacteria can exacerbate insulin resistance and PCOS symptoms. I strongly suggest testing instead of guessing by working with a skilled practitioner to analyze what is going on in your specific gut. Again, spot treating by throwing probiotics at the problem is not going to FIX anything. However we can eat to support a healthy gut. It’s actually quite simple, it’s not some elaborate crazy diet plan. Simply eat whole foods that mostly come from plants – vegetables, beans, nuts, whole grains, fruits and eat a variety to give your gut a diverse amount of fiber. The rest of the plate can include healthy meat, fish, poultry and eggs. You can try starting with ¾ of your plate being plants and the rest being protein. Keep in mind we need healthy fats like avocado, nuts, seeds, olive oil, coconut oil and animal fat to round out the meal and keep our blood sugar stable.EAT FOR YOUR HORMONES
Does it surprise you to learn that your digestive tract needs 12 hours to heal? Eating all the time keeps your digestive system awake and working around the clock which is not great for your PCOS. One thing you can try is eating within 1 hour of waking preferably by 7am – 8am, then having lunch around 12pm – 1pm and finishing dinner between 6pm-7pm. This allows 12 hours for your body to be in a fasting mode. Finally, another thing to try would be to eat a larger breakfast and smaller meals for lunch and dinner. To be clear, this suggestion is not a calorie restriction. In fact there is a recent study that found obese women who ate ½ their calorites for breakfast, ⅓ for lunch and another ⅓ for dinner lost 2.5x more weight, had better insulin levels, lower triglycerides, and felt less hungry.There are additional steps you can take to support your PCOS like avoiding endocrine disruptors, exercising, managing stress and working with a knowledgeable practitioner who can help you with some of these intricate choices.
PCOS is a lot, there is not a cure but there are definite lifestyle interventions that can knock back the symptoms and the downstream issues in a huge way. PCOS can be managed in a healthy way if you know what to do. If you should need any additional assistance, please feel free to book a 20 minute consultation with me and I’m happy to discuss your PCOS with you.
There are additional steps you can take to support your PCOS like avoiding endocrine disruptors, exercising, managing stress and working with a knowledgeable practitioner who can help you with some of these intricate choices.
PCOS is a lot, there is not a cure but there are definite lifestyle interventions that can knock back the symptoms and the downstream issues in a huge way. PCOS can be managed in a healthy way if you know what to do. If you should need any additional assistance, please feel free to book a 20 minute consultation with me and I’m happy to discuss your PCOS with you.
